|
|
 |
|
 |
 |
|
 |
|
 |
|
 |
|
 |
|
Not enough people are aware of the stunning achievements that Bangladesh has recorded in improving the health of its citizens. Zakir Hossain discusses the dedication and commitment that have gone behind the improvements in the health sector and have touched the lives of every single Bangladeshi.
In sickness and in health
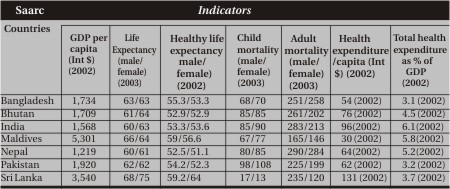
The table above shows the achievements of the Bangladesh public health service interventions as per the World Health Report of 2005. The indicators in life expectancy and child and adult mortality evidence very aptly where Bangladesh stands among the Saarc countries (in 2002-2003).
There are two pertinent issues that need to be flagged. One is the more or less indistinguishable difference between the sexes in the health status and the other one is the efficiency with which Bangladesh has achieved these milestones.
With a per capita health expenditure of only 54 international dollars, the lowest in the Saarc region, and with a total health expenditure that is only 3.1 percent of GDP, again being the lowest in the region, Bangladesh stands behind only Maldives and Sri Lanka in terms of the most important public health indicators.
Efficiency-wise Bangladesh's achievements are therefore arguably the best. A trend in these and some other indicators are shown below.
The facts and figures are testimony to how Bangladesh has and is emerging fast as the most efficient and effective country in the region in reaching the desired health status of its population. How was this achievement made possible?
Strengths: How was this feat possible
Bangladesh is a homogenous society: culturally, linguistically, and geographically, barring some minor variations. Its population is quite democratic attitudinally and looks for avenues through which the people can exert their rights. Through a public educational system and social network people have learnt further and quite quickly about the value of health in social and economic development. Bangladesh's health and population-based infrastructure is extensive and arguably more functional than many of the other countries in the region. Both its public health sector and non-governmental organisations are appreciably dedicated and committed, despite some scathing criticism, specially against the public sector.This dedication and commitment are reflections of some individual patriotism, dedication, and commitment. The government health sector itself, however, is also keen to learn and quite accommodative and tolerant to criticism. It is also unflinching in its approach to test and adopt new ground -- systems, approach, policy, strategy, and program, albeit this is not always pragmatic.
Social dynamics, solidarity, and camaraderie are quite appreciable in Bangladesh. The communication system has improved at a rapid pace since independence which has expedited health services when it comes to reaching areas better than before. Planning and implementation skills have improved with time.
More managers are keen to see the result of their efforts. Managers are more knowledgeable about the national priorities and more managers keep themselves abreast of the latest information and health indicators. Exchange of ideas and innovations are more frequent. Program reviews are more regular. Management instructions are channeled better to the lower levels. Smaller and more frequent successes have bolstered the confidence and pride of the service providers.
There is better collaboration and coordination with the potential partners and allies and better use of the available resources, i.e., partners like non-governmental organisations. Quantity-wise more training programs are organised, which at least have some effect. More logistical support is available and more funds are given from the public exchequer for program implementation.
One of the reasons that the health sector has achieved the health related goals in recent times is the fact that the first two five-year development plans did not include any budget for the health related activities (they were only population plans). It was only since the third population and health plan (1987-1992) that health related activities were included in the development plans of the health sector, and budget was allocated accordingly. In the light of this reality also the health related achievements are quite laudable.
Weaknesses: Why more could not be achieved
Although not unique to Bangladesh, there are frequent instances of excess paper work in the form of drafting of strategies and plans and training programs that are undertaken without any sustained purpose and follow up. Many of these end up in shelves to gather dust and do not see the light of the day. Much needed funds, time, and energy go astray, as such. Many a times these are undertaken because there are some funds available for the purpose and there is some donor priority, which obviously does not match with that of the program on ground (not all relevant donor personnel are really very relevant for a given program).Human resource development activities are not always need based or task and job oriented. Staff deployment does not follow required skill mix. Personnel management is weak. There is no incentive or disincentive system. Political interference on the other hand, makes the situation worse. The logistics and management information system are abysmal. Personal predilection in human resource development, deployment, and logistics procurement override the actual need, and hence no well-organised formal system of need assessment and institutional development in these areas has taken solid root yet.
Evaluation and research work do not feed into policy and management decisions, and in fact most of them are either clinical or repetitive, not so original, or tailor-made, and are hardly requested for by the policy makers or managers themselves. The conducted research findings are of no use for improving or strengthening the medical, nursing, or paramedical educational or training systems or their service and management qualities.
There is lack of transparency in the financial and procurement (service, construction, or goods) systems. Separate budget for development and revenue programs is one avenue, but the more cogent reason is poor financial allocation, planning, and tracking system. These do not commensurate with the needs, particularly of the poor and the vulnerable.
The audit system itself is questionable. Supervision and monitoring is yet another very weak area. Not enough attention is given in the plans for this very useful function which is important for the success in implementation of a plan. There are opportunities which the bureaucracy and technocracy has failed to seize. Implementation of programs is sluggish and fails to utilise the available allocations. One of the reasons of this is lack of understanding on the part of many of the managers of the plan and lack of ownership of the same by the managers, and also poverty of planning and management capacity, disorganised or absence of formal and well-organised review and evaluation functions.
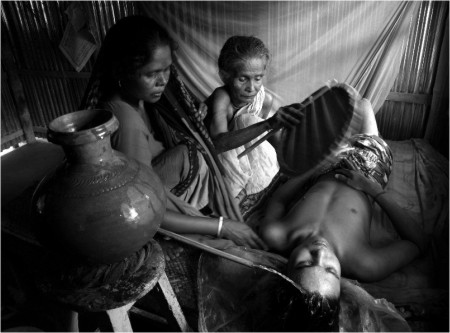
There is a gap between the service providers and service recipients and the reasons thereof may be very effectively summed up in the language of a service recipient, which goes like this: “The physicians should stay in the upazila hospitals for providing health services and they should be given good accommodation, social security, and attractive incentive package.” (Extract from a dialogue held in Chittagong by the Development Organisation of the Rural Poor on October 16, 2004, page 35 in Health in Poverty Reduction Strategy: Bangladesh Perspective, Meso Situation Report 2004).
Opportunities
One of the strengths and also weaknesses, especially in the health sector, is that it sits on a treasure trove of documents -- policies, plans, and strategies on different programs, e.g., the sector as a whole (health policy and population policy), HIV/Aids, tuberculosis, disaster management, reproductive health, communication, etc. Many of the relevant officials are oblivious of the existence of these documents and most do not take interest in the contents of these documents. Many even do not really understand them.The health sector reform that was undertaken under the rubric of Health & Population Sector Strategy and the Health Policy have given, despite all their criticisms, at least three boosters to the sector -- one is the line directorship which has made program implementation duplication free, and therefore more efficient, by the dint of this reform alone.
The second is the decentralisation, albeit limited in scope, which has given some leeway to the local level managers to address some of the issues that are unique to the locality in a more appropriate way, if not in an adequate way yet. This needs to be scaled up further in a graduated degree, based on the experience garnered so far.
The third one is the construction of community clinics, which was an effort to take the health care service structure closer to the people in general, and the poor in particular, who refrain from seeking health care mainly because of the opportunity cost that is involved.
The information system that Bangladesh has for the health sector is quite appreciable. While most of the health sector information in the regional and neighbouring countries comes from the public sector, except for the Demographic and Health Survey conducted through USAID funds, in Bangladesh there are many independent surveys which generate more valid data than the data that come from the public sector. In that sense the data that we have in Bangladesh arguably is of higher quality. So we know better where we stand and how far we need to go.
Caveats
Donor representatives in Bangladesh have to account for their policy, strategy, program thrust, and allocation to their respective government. At times they have to abide by the policies and priorities of their own governments. Relevant officials in Bangladesh have to understand that to exploit the situation to their advantage.At times, however, due to lack of political and/or technical understanding of the country situation, the donor representatives might fail to take a correct avenue. Public sector officials need to be smart enough to guide them well. Otherwise there are others who might take advantage of this situation to the detriment of the public sector.
Non-public sector performance is more effective, but probably less efficient. A collaboration with changed roles between them may change this to a function that would be more effective and at the same time more efficient. Since there has been a new trend on the horizon now of channeling donor funds to the non-public sector through the public sector coordination and leadership, this condition of providing more effective and efficient services is on the cards.
There is also a new emphasis on getting things done by the donors through multilateral agencies instead of non-governmental agencies in Bangladesh. The public sector needs to assess how effective and efficient that would be. Relevant government offices and officials have to rise to the occasion and prove their worth of leadership.
Future direction
1. Emphasise on nutrition, public health, sanitation, and communication for behaviour initiatives (prioritise those disease control programs that maximise economic benefit, e.g., EPI, tuberculosis, HIV/Aids/-STI/STD, malaria, diarrhoea, malnutrition, etc.) with the cardinal aim of changing the way people look at the disease and health issues and status, and also to change the health seeking behaviour of especially the poor and the vulnerable.2. Prioritise and improve the national budget on health, education, and communication, and allocate on the basis of population size and poverty index geographically, keeping the Millennium Development Goals in the forefront.
3. Undertake effective communication to orient the service providers to the role and rights of the public and also sensitise the public, specially the vulnerable, about their public rights.
4. Improve the voice of the poor, women and children in the management of the health sector and ensure civil society/service recipients' role in review, monitoring, and planning of health sector programs.
5. Institutionalise maintenance, review, supervisory, monitoring, and expenditure tracking functions in the sector through a strong performance and financial management information system (allocate sufficient budget for maintenance -- about 15 per cent of the capital cost).
6. Institutionalise system of incentives to achievers.
7. Keep the politicisation of the health sector under leash (it is a double-edged sword) and improve governance issues.
8. Change the public sector role -- it should be an efficient steward and contract manager rather than service provider. Service provision should be left to the more accountable. It needs to strengthen its planning and contract management capacity, specially the economic and financing mechanism, allocation, tracking and expenditure capacity and human resources management/personnel administration. This ought to be the most important facet in coming days. Experience may be gleaned from the Asian Development Bank and co-financier funded Urban Primary Health Care Project.
9. Strengthen management structure and functions and create a seamless understanding by the managers of the existing relevant public documents. Some sort of coaching and training are warranted for this. Effective steps need to be taken to improve quality (effectiveness) of training. Change is needed in the way trainings are conducted and followed up.
10. Establish effective liaison, collaboration, and coordination with other relevant development agencies and ministries, e.g., education, religious affairs, information, and agriculture, in order to use their facilities, logistics and strength and vice versa. This has to be further stretched to the collaboration with global partners and funders, as funding is becoming more stringent.
11. Establish and institutionalise equity equally in input and outcome, and develop a tracking system to monitor input and effect/impact equity. This needs the establishment of strong operational research wing at the directorates level (or make use of the existing infrastructure for this purpose).
12. Make the best use of the available health care facilities and agencies, including the non-governmental organisations and the community clinics, not for only for providing health care but also as a bastion of overall community development activities.
13. Establish close programmatic collaboration and coordination with the Ministries of Education, Religious Affairs, Agriculture, and Information.
14. Ensure environmental sustainability of the development projects.
15. Make use of the health sector personnel for overall socio-economic development, earning and education in particular, so as to enhance health buying capacity of the people.
....................................................
Dr. Zakir Hossain is Managing Director of Partners in Health & Development and ex-Director of Primary Health Care & Disease Control, Directorate General of Health Services, Ministry of Health & Family Welfare.