Inside
|
No Child Left Behind Shumon Sengupta believes its time to act now, if young lives are to be saved. Every child is precious and every child has the inherent right to life. Everyone of us parents, care-givers. Government, NGOs, civil society, the media and even the man on the street has the responsibility to ensure that every child survives.
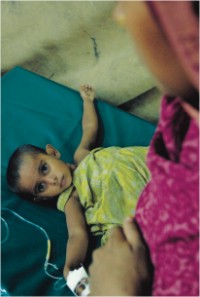
In Bangladesh, 244,000 children die yearly before reaching their 5th birthday, primarily from causes that are easily preventable. They die of diarrhea, pneumonia, complications in newborns etc., often complicated by malnutrition, etc. conditions that we can now treat but were once deadly. So in theory, we can now save 28 Bangladeshi children every hour. The question is, how? The revolution to save lives The Declaration notes that attaining the highest possible level of health "is a world-wide social goal whose realisation requires the action of many other social and economic sectors, in addition to the health sector." What followed this declaration closely was a Unicef-led, more practical approach to saving newborn and child lives. Given the limitations of our resources and commitments, more selective and practical primary health care packages were proposed that prioritised smaller, more attainable health objectives. And this did save millions of lives. While the child survival revolution did focus on appropriate, life-saving technical interventions, it did not adequately emphasise on the need to address the underlying social, political, cultural, institutional and economic determinants that contribute to new born and child mortality, particularly in developing countries. It is therefore not surprising that there has been rising levels of malnutrition and slow decline in infant and child mortality rates in many countries because real per capita government health expenditures have actually declined or remained alarmingly low in many countries. Why now? But tragically, the fact remains that across the world, in 2009 over 9 million children will die from disease and causes we can treat and prevent. Moreover, recent world events have made reaching the MDG targets seem even more unattainable. According to Save the Children estimates, it's children in the developing world, including Bangladesh, who are most vulnerable to the effects of climate change, rising food and fuel costs have already forced millions more families into poverty, and could undo decades of progress and most alarmingly, the global financial downturn threatens to hit the children in the developing world hardest and put even more children's lives at risk. However, the good news is, politicians and donor countries have become more aware of the issue. In the case of Bangladesh, significant progress has already been made with respect to lowering child mortality with successive governments becoming more aware of the life-threatening implications of inequity and poverty. Bangladesh is now a flourishing democracy with a conscientious voting republic who have always voted for progress. Bangladesh also has a government which is committed to making Bangladesh a middle-income country by 2021. Therefore, now is the time to ask for a healthy, thriving Bangladesh that will drive us to 2021, a Bangladesh where over 175,000 children's lives are saved yearly. Bangladesh -- a success story Demographic and Health Surveys (DHS) conducted between 1990 and 2001 in Bangladesh, India, Nepal, and Pakistan, Cambodia, Indonesia, the Philippines, and Vietnam found that child survival is indeed improving in the Asian region. However, out of these eight countries, only three countries have brought under-five mortality down to less than 70 deaths per 1,000 live birthsVietnam, the Philippines, and Indonesia. Under-five death rates came down by approximately 4 percent a year in Bangladesh, 2 percent in India, 5 percent in Nepal, 9 percent in Indonesia, and 2 percent in the Philippines and the good news is that if these rates of improvement can be maintained, Indonesia, Nepal, and Bangladesh will meet the Millennium Development Goal (MDG 4) of reducing under-five mortality by two-thirds over the 25 years from 1990 to 2015. The bad news is -- India and the Philippines may not. Immunisation against six fatal but easily preventable diseases--tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, and measles --is one of the most cost-effective interventions available to national health systems and full immunisation rates are high in Bangladesh, which is a significant achievement of the country's health system. Diarrhea and neo-natal causes, complications arising during the first year of birth are the most important killers of young children .
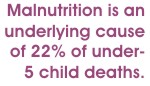
When a child suffers from diarrhea, the treatment includes giving increased fluids plus a solution made from clean water and an oral re-hydration salt (ORS) packet. A homemade re-hydration solution is sometimes administered if the packets are not available easily. In Bangladesh, more than four out of five children who were ill with diarrhea during the two weeks before the survey were given at least one of the recommended oral re-hydration treatments. The International Center for Diarrheal Disease Research, Bangladesh (ICDDR,B) invented oral re-hydration therapy more than 30 years ago, and the Center, Government and other groups have been working actively and very successfully to educate Bangladeshi mothers on diarrhea prevention and treatment. This is yet another major achievement for Bangladesh. However, behind the overall success story in Bangladesh, of which every Bangladeshi ought to feel proud, are certain lingering concerns that the country will have to address sooner rather than later, in order to ensure that it remains on track on MDG 4. Bangladesh for example has particularly low proportions of women giving birth with assistance from trained personnel and fewer than one in 10 deliveries occur in a health facility. This surely needs to improve. Globally, acute respiratory infection (ARI), primarily pneumonia, is the most important cause of death among under-five children. The symptoms of ARI are cough accompanied by short, rapid breathing and it is imperative to take the child with these symptoms to a health facility for timely diagnosis and treatment with antibiotics. Sadly, the percentage of such children taken for treatment is much lower in Bangladesh compared to many other Asian countries, and Bangladesh needs to address this gap urgently. Good nutrition is a major determinant of a child's health and well being and unfortunately, there is widespread child under-nutrition in Bangladesh. Malnutrition is an underlying cause of 22% of under-5 child deaths. In terms of weight for age, a composite measure that takes into account both long and short-term under-nutrition, four to five out of every ten children under three years of age are undernourished. More than one out of 10 children under age three is severely undernourished and this is alarming. Public expenditure on health also makes a critical difference. The two countries with the lowest under-five mortality rates Vietnam and the Philippines spend the most per capita on healthcare. The Philippines spent US$167 per capita in 2002, and Vietnam spent US$130 in 2003). In contrast, Bagladesh spent barely US$47. This is clearly an area for policy change. Further, although Bangladesh is on track on MDG 4, there still exists an incidence of inequity in terms of access to health services in the country both with reference to household's economic status and geographical locations. Incidence of new born and child mortality is highest amongst the poorest 20 % of the population and in certain remote geographical locations. Save the Children UK's director of policy, David Mepham said: "A child's chance of making it to its fifth birthday depends on the country or community it is born into. This sounds like a lottery, something beyond human control, but this should not be the case. While poverty and inequality are consistent underlying causes of child deaths, all countries, even the poorest, can cut child mortality if they pursue the right policies and prioritise their poorest families. Good government choices save children's lives but bad ones are a death sentence." Bangladesh has already made significant progress in this regard. In 1998 the government put its resources and its political weight behind a national initiative to tackle childhood illness and reduce levels of fertility. Ten years later that policy decision has paid off. Bangladesh, despite its relatively low Gross National Income (GNI), is one of the few countries on track to meet the child survival Millennium Development Goal - to reduce the number of children dying before their fifth birthday by two-thirds by 2015. Access to free, and quality primary health care - particularly for the poorest 20% of the population is therefore a priority for the health system in Bangladesh. For the poor in the country, the safe delivery of a healthy child and the survival of both mother and child cannot be taken for granted and hence achieving equity in health services is extremely important. Let's talk about it The importance of this achievement in the long term development of the nation needs to be appreciated and celebrated by the citizens at large. It will send a very strong feedback to the government that the public appreciates and values this achievement and sees it as an important development issue for the country, which will in turn motivate and inspire the government in keeping the momentum up and address the gaps discussed earlier. On the other hand, there is an equal lack of adequate public concern and discourse on the fact that large number of children are still dying from easily preventable causes or are going hungry and suffering from malnutrition and under-nutrition. The lack of a public discourse on this issue is undermining what the general public and non-state actors can do to support the government in these areas. The need for popular engagement The engagement of the populace aims to facilitate such public discussion based on interactive public reasoning an exercise which we need to constantly engage in. According to Sen, public discussion and deliberation can lead to a better understanding of the role, reach and significance of particular functioning and their combinations. In a democracy, every child must be regarded as indispensable and it is the failure of the society at large to prevent deaths of children and mothers. Unfortunately, the issue of children's health seldom finds space in contemporary social and political discourse in south Asia in general, including Bangladesh. The process of ensuring that every child is taken care of as a matter of basic right involves societal concern expressed through public action. No democratic society tolerates iniquitous access to services in health and nutrition and has little care for the respect and well-being of its infants and mothers. In South Asia (with the notable exception of Sri Lanka) pregnancy, delivery and new born survival are fraught with risk among the poor. There is a high degree of passive acceptance to fate, I am poor, therefore my child will die-- despite the fact that the risks can be reduced and deaths can be prevented very easily. This attitude unfortunately cuts across classes and is so pervasive that there is overwhelming complacence.
A wide-spread social norm that supports the well-being of women and children is highly likely to positively influence the state and non-state actors in the country to take up their responsibility towards the survival of mothers and children. Some of the contentious areas that need to be discussed and debated through public discourse and reasoning include the modalities for concretising delivery mechanisms for health care; the ways the country can afford millions of trained professionals to take care of its children and over the need for professionalism and human resource development in the health sector. The issues of linkages between the public and private service providers, the contentious issue of privatisation/outsourcing of health care services, health equity versus user charges, how the private health sector may be better regulated etc are among the important topics for pubic discourse and debate. Issues such as increasing health budgets, investments in paramedics and community health workers and participation of alternate health care providers versus professional support to the poor also need to emerge in public discussion. Such a public discussion, facilitated through popular mobilisation and conducted on the basis of public reasoning will go a long way in supporting the government in making the right and acceptable strategic and policy choices. Popular mobilisation of such a nature will also increase the demand for improved governance and better service delivery and equity. In a progressive democracy such as Bangladesh's, citizens are ultimately morally responsible for the actions of their government. The populace's participation and public discourse will facilitate mechanisms that will integrate officials, governmental organisations, non state actors and individual initiatives to assume collective responsibility for the effective functioning of the health system and improving new born and child survival in the country. It could also potentially enhance accountability and ensure credibility with international donors who are investing in the country. Experience shows that institutions and systems do not operate in a vacuum and are not always self driven. Policies and institutions for the weakest, such as the health policy and health care system for the poor become more effective and vibrant when the processes of policy and institution building has strong interface with citizens and there is active participation intellectually, morally as well as in practice with the public. While the original "child survival revolution" essentially emphasised on applying a rather technological solution to outstanding health problems, it did not focus on the equally critical political, social, institutional and economic determinants that lay beneath the health problems. Citizen participation through public discourse and reasoning will bring maternal, newborn and child health into the very centre of the development debate and address the political, social and institutional determinants of new born and child mortality. Participation, one of the pivotal pillars of good governance and democracy, could potentially encourage strong and enlightened national and local leadership to develop appropriate health policies, design health systems, promote health equity, facilitate partnerships and develop a collective responsibility for health. It would also help discuss and address some of the underlying social, cultural and economic determinants of new born and child survival. While it is important that we continue to increase coverage of key interventions which can save children's lives, ultimately, it is through the participation of all citizens the policy makers, the youth, the civil society and the media, the health professionals and the affected families that we can create an environment for social and political change where more and more children will live to celebrate their fifth birthdays. So we know how to save children's lives. Why don't we? Shumon Sengupta is Country Director, Save the Children UK
|