Inside
|
Every Life Counts Nazme Sabina examines if we are on track to achieve MDG-4, reducing child mortality In 2000, governments around the world committed themselves to the Millennium Development Goals (MDGs), eight targets revolving around international development including education, health and gender equality. MDG 4 is specifically focused on child survival, calling for a reduction by two-thirds in the number of deaths of children under five. To achieve MDG 4, Bangladesh must reduce under-five mortality, from 151 deaths per 1000 in 1990 to 50 by 2015, and infant mortality rate, the number of children dying at or under the age of one, from 94 deaths per 1000 live births in 1990 to 31 by 2015. The third target is to enhance the proportion of immunised one-year-olds for measles from 53 percent in 1992 to 100 percent by 2015.
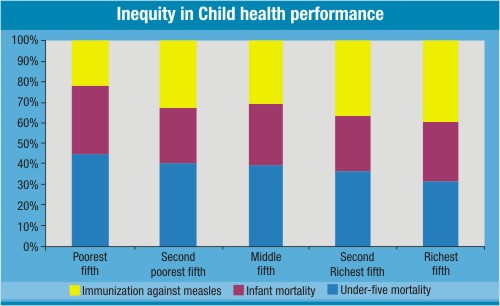
According to the latest MDG progress report, the more pronounced causes of infant and child mortality are diarrhea, pneumonia, infection etc. However, there are other intermediate causes like poor nutrition, maternal literacy, lack of access to water and sanitation, etc. and structural issues such as poverty, inequality and exclusion, climate change and natural disasters, and global political economy. All these factors globally contribute to the deaths of over 9 million children, under-five every year. It appears from the Bangladesh Demographic Health Surveys (BDHS) that the achievements of Bangladesh in reducing child mortality are very encouraging: under-five mortality decline by almost half, i.e. at an average rate of 5.3% per year which exceeds the required annual decline of 4.3% needed to achieve the Goal. The levels of coverage for BCG and the first two doses of DPT and polio are close to 90 percent or above. Measles vaccine rates at 76 precent are much lower though. The trends noted above may look promising. The caveat, however, is that the improvements are based on overall trends at the national level. However, things would look quite different if we put on our "equity" lenses and looked at the socio-economic and geographical dis-aggregation of this data. Poverty, though, indirectly remains an underlying cause of child deaths in Bangladesh. Consistently, we see that it is the children in the poorest households and in the poorest communities who are dying. The BDHS data also suggests that the children of poorest households are more likely than their better off peers to die within the first five years of their birth. In the richest group, the child mortality rate is 72 per 1000, and in the poorest group, the rate is a staggering 121 per 1000. Although the poorest-richest ratio has been improving, the poorest are not getting benefits for reduction in mortality. Children in the richest fifth households are more gainful than their poorest peers in measles vaccination-- 90 percent children from the highest wealth group and 60 percent from the lowest wealth group are vaccinated for this disease. Interestingly enough, mortality among rural children is much lower than that of their urban peers over the years. This difference is explained by the thrust or focus put in rural areas by health programs. The urban rates may reflect the lowest levels achievable with existing programs at current coverage levels. This may mean that the recent decline in overall under-five mortality may not be easy to sustain. The measles vaccination coverage is nearly 10 percentage points higher compared to rural areas. Again, different geographical areas of Bangladesh portray different scenarios. The divisions with highest mortality in under-five, infant, and neonates are also places that belong to the lowest poverty line in Sylhet, closely followed by Barisal. The performance of these indicators is also low in hard to reach areas like haor regions, Chittagong Hill Tracts, and the coastal districts. Mortality rates among girl children aged between 1-59 months have been declining faster than among boys. The overall under-five mortality rate is almost 10 points higher for boys than for girls, largely due to much lower neonatal mortality among girls, which is the norm of low mortality populations, such as ours. However, there exists a gender disparity in our child mortality accounting that the overall national figures may not be entirely reflective of. Therefore, the national average is not necessarily reflective of the various wealth, gender and geographical differences that exist in our progress towards achieving MDG 4.
The relationship between the MDGs The relationships are all intricately related and work on many folds. Families' level of income, wealth, mother's education and health whether they can afford transport to the health facilities and whether mothers can decide on economic and financial issues, affects children's health. The growth, development and ultimately the survival of a child depends on his/her primary care-giver -- the mother. One of the most powerful indicators of this is the relationship between child mortality and mother's education. Under-five children whose mothers have no education are 40 percent more likely to die than those whose mothers have at least a secondary education. A number of factors linked to mothers' education and empowerment influence child mortality since education exposes mothers to information about better nutrition, use of contraception to control births, childhood illnesses and their treatment, and additionally it improves women's earning potential, which in turn can also contribute to a more nutritious diet for mother and child. Furthermore, empowerment and gender equity improves women's bargaining power within the household. In all senses of the term, empowered mothers are necessary to raise healthier offspring. Poverty again is a stumbling block to woman's empowerment. Poor people can hardly afford safe drinking water, sanitation and hygiene facilities. Low income primarily accounts for two consequences: it enhances the chances of hunger and malnutrition, for example, people are unlikely to afford the diverse diet necessary for good complementary feeding; thereby reducing resistance to disease. Secondly, it constrains the usage of appropriate medical care, both directly as medical fees cannot be paid, and indirectly as transport and the other costs associated with using health services are not affordable given the high 'opportunity costs; such as income foregone owing to the time spent seeking healthcare. Moreover, poor people live in geographically hard to reach and disaster-prone areas where doctors and nurses are absent, supply of drugs are inadequate, and X-ray and other equipments are unable to function. These deprivation effects on child health can be reduced by well-designed policies, programs and popular mobilisation--the three necessary Ps of a successful, national child health campaign.
Staying on track Cash transfer mechanism can be introduced to make health care affordable to the children of poor families. Since income poverty is a key driver of other poverty outcomes, such as poor health and nutrition, cash can empower poor individuals and households to make their own decisions in improving their lives. Increasing demand for services, bringing about changes in behaviour and practices on health and empowerment issues, for example, promotion of exclusive breastfeeding, good complementary feeding practices, women's education, birth registration, maternity and child benefits could be the messages for people from all walks of life. This will be a public-health gain, which can be brought about by the synthesis of social, political and policy change. Improvements of knowledge and changing of behaviour in terms of improving newborn and child health is not enough. We need to bring sustained changes in the perception of people, and above all, commitments to remove inequity in child health. These can only be achieved if the citizens of the country alongside the policy makers recognise that child survival is an issue we can no longer afford to be complacent about. Both targeting and universal coverage have strengths and weaknesses. The people at the helm of designing development program and policy makers alike should give serious consideration to both concepts to improve equity in child health. Progress at the macro level, but leaving poor people, women, or geographic minority groups behind in the process is neither enough nor fair. Taking all of the above, one needs to link different MDGs together--which is a matter of policy translated into program. Development partners, including the government, need more holistic policies to sustain the achievements. Moreover, detailed, scaled-up, national-level program are needed to reach the unreachable, where they need health services the most. In so doing, we are not asking for money or other resources rather stressing upon the commitment of the society and its actors. Let us realise that these are our agonies to endure and our agendas to pursue. Let us ensure that healthcare facilities are available where the poor children live, and overcome their social, cultural and economic barriers to access. .
Often times, though we see monumental changes in policy, change does not get translated to all strata of society. In order to be able to save over 175,000 children yearly, by 2015, we need more than health programs and policies. We need every one to recognise that being on track to achieving MDG 4 is not the end staying on track, for now and for always is what is desired. Nazme Sabina is a development economist. |